Abstract
Background: haploidentical hematopoietic stem cell transplant (HSCT) with post-transplant cyclophosphamide (Cy) is a procedure for patients with advanced haematological malignancies lacking an HLA identical donor. Even if several groups reported interesting results about allograft in lymphoma, the current clinical practice doesn't include routinely allogeneic stem cell transplantation in patients with suboptimal response to salvage strategies.
A prospective study based on the use of peripheral blood stem cells (PBSC) as graft source was launched at European Institute of Oncology in 2010. The aim of this paper is to report the results of haplo-HSCT in patients with relapsed and refractory lymphoma with detectable disease before transplant.
Patients and Methods: between June 2010 and May 2018, 64 have been enrolled in the study at our institute; the updated experience of 35 patients affected by high risk lymphomas is reported.Haploidentical HSCT was performed with G-CSF mobilized PBSC. Conditioning regimen was either non-myeloablative (31 patients) (Cy 14.5 mg/kg/die days -6,-5, fludarabine 30 mg/m2/die days -6 to -2, and 200 cGy Total Body Irradiation day -1), or myeloablative (treosulfane 14 mg/m2/die days -6 to -3 and fludarabine 30 mg/m2/die days -6 to -2). GVHD prophylaxis consisted of post-transplant cyclophosphamide (50 mg/kg day +3 and +4) and mycophenolate and tacrolimus as previously described.Among 35 evaluable patients, 28 (80%) performed haplo-HSCT for refractory/relapsed non-Hodgkin lymphoma; the remaining patients included 7 relapsed and refractory Hodgkin lymphoma. Median age was 52 (19-73), disease status included 13 (37%) complete remission (2 CR1, 11 CR≥2), 9 (26%) partial response (PR), 4 (11%) stable disease (SD), 9 (25%) progressive disease (PD). A median of 5.5 x106(range 2.45 -13.4) CD34+ cells/kg was infused, with a median of 2.8x108(range 0.3-5.4) CD3+ cells/kg. Median lines of previous treatment: 3 (0-7).
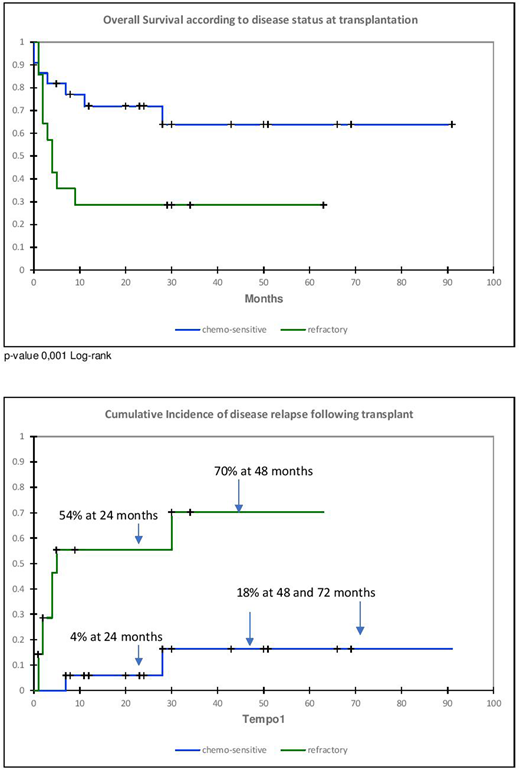
Results: four deaths due to infections have been recorded before engraftment. Among all 64 evaluable patients, median time to absolute neutrophils ≥500/µL was 18 days (range 12-29), and 23 days (range 11-65) to platelets ≥20.000/µL. Incidence of grade I-II acute GVHD was 22%, with grade III of 2%. Mild chronic GvHD was observed in 7/60 evaluable patients (1-year cumulative incidence: 13 %). Mixed donor chimerism was achieved in all 60 evaluable patients, with CD3+ chimerism >50% at day +28, >90% at day + 84. No graft failure has been recorded. CMV reactivation occurred in 77% of lymphoma patients (27/35 subjects at risk), at a median of 35 days (range 5-50) post-HSCT; pre-emptive therapy was effective in all patients. Regarding the lymphoma population, with a median follow-up of 360 days (6-2,460), 19 patients are alive (54%), 18 of them (51% of the whole series) in CR, while the cumulative incidence of relapse is 25%; when disease status at transplant is considered, the incidence of relapse at 2 years is 4% and 54% for chemo-sensitive and chemo-refractory, respectively (see graphic 2 in figure 1). Overall, 16 patients (45%) died; causes of death were PD in 8 patients (50%), infections in 8 (50%) with a cumulative transplant related mortality of 45%. The 3-year PFS and OS for the all lymphoma patients is 58% and 54%, respectively, with 81% and 66% for patients transplanted in CR/PR and 32 % and 31% for those transplanted in SD/PD (p-value 0,001 Log-rank - graphic 1 in figure 1).
Conclusions: Haploidentical T-cell replete PBSC transplantation with high-dose post-transplant Cy is a feasible procedure for high-risk haematological malignancies, with an overall toxicity analogous to HSCT with HLA-identical donors. Despite the small study population, haplo-HSCT seems to be an effective strategy even in patients with active lymphoma before transplant. As previously reported, chemosensitive (CR/PR) patients have a better outcome compared to chemo-refractory cases. However, the latter population still may have a benefit from haplo-HSCT as suggested by our data, thus the cellular therapy strategy should not be discouraged in presence of disease (SD/PD). Our future purpose is to enhance the graft versus lymphoma effect with Natural Killer cells infusions. This option will be soon developed at our hospital within a prospective trial.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal